Age-Related Macular Degeneration (AMD)
Age-Related Macular Degeneration (AMD) is a disease of the macula, the central part of the retina. As the name suggests, it is a degenerative condition and is currently one of the leading causes of blindness in our environment.
This disease typically affects patients over the age of 50 (specially over 80) and does not show a preference for either sex. Additionally, it has been found to be more common in smokers, people who have worked in the sun their whole lives, or those with unbalanced diets.
The main symptom of AMD is a decrease in visual acuity (i.e., blurred vision), which worsens as the disease progresses. This vision loss is typically central – patients always retain peripheral vision; only the central area is affected. Moreover, at a certain stage, especially in one subtype, distortion of shapes often occurs. This phenomenon is known as metamorphopsia.
Therefore, in the later stages of the disease, central vision can become very limited, but patients are not completely blind. They still see with their peripheral vision, so they’re not “in the dark” or bumping into furniture. However, reading, recognizing faces, and performing precise tasks becomes increasingly difficult.
Contents
Initial Dry Age-Related Macular Degeneration
This subtype is characterized by slow progression. Material produced by the degeneration accumulates in the retina, and little by little, over the years, the patient gradually loses vision. Shape distortion usually only appears in very advanced stages.
A balanced diet, not smoking, and regular check-ups are fundamental for these patients. Also, due to the older age of onset and slow progression, many patients never reach the terminal stage of the disease.
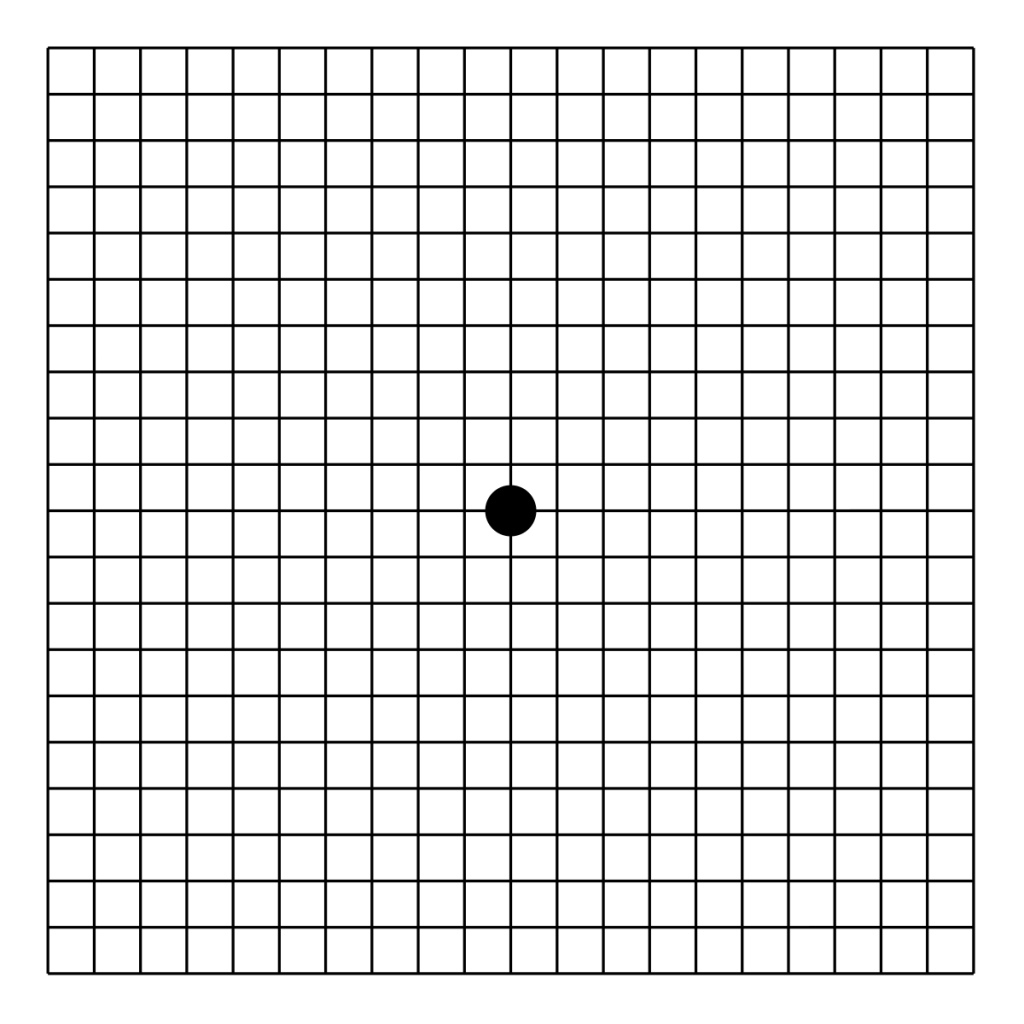
It is recommended to visit the doctor every 6 to 12 months if there are no new symptoms. However, a simple home check can be done using grids or patterns to ensure they don’t appear distorted. A useful option is to print an Amsler grid (there’s one at the end of the article), stick it on the fridge, and test your vision with it once a week.
Few treatments have been proven good results for initial or intermediate AMD:
-Vitamins: to help the patients reach a balanced diet with all the necessary vitamins.
–Photobiomodulation: a laser stimulation of the retina cells
-Pegcetacoplan: an intravitreal injection. However, this has been rejected by the European Medical Association (in contrast to the FDA) due to its risk/benefit ratio.
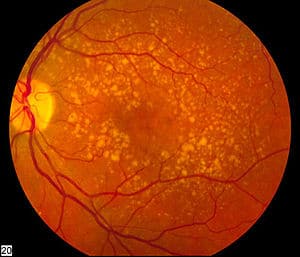
Atrophic macular degeneration, or advanced dry AMD, is the final stage of the dry form of age-related macular degeneration. At this point, the retina – and more specifically, the macula – shows visible signs of geographic atrophy, meaning areas of the tissue have died and are no longer functioning.
This condition causes a permanent and irreversible loss of central vision. Unlike the early or intermediate stages, where drusen buildup and mild cell damage are the main issues, in atrophic AMD the photoreceptors and supporting cells (RPE and choriocapillaris) have completely degenerated. This leads to dark patches or blind spots in the center of the visual field. The damage can start small but often expands gradually over time.
Patients often notice that reading, recognizing faces, or watching television becomes extremely difficult or even impossible. However – and this is important – peripheral vision is preserved. So while the ability to see fine detail is lost, patients are not completely blind and can usually navigate familiar environments.
Currently, there’s no treatment that can reverse atrophic AMD. However, research is ongoing, and some clinical trials are exploring new drugs aimed at slowing down the spread of atrophy.
In the meantime, regular monitoring, low vision aids, and adaptations at home can help maintain independence. Simple things like magnifiers, electronic readers, and brighter lighting make a big difference. And as always, controlling risk factors – especially smoking – remains essential.
If you’re living with dry AMD, it’s important to stay in touch with your eye care team. Catching progression early may help you benefit from new treatments as they become available.
Wet Age-Related Macular Degeneration
This subtype is characterized by rapid progression. It can appear spontaneously or in a patient who already had dry AMD. In this disease, a new lesion forms — a neovascular membrane. This membrane, made up of blood vessels, leaks fluid and ends up deforming the retina from underneath.
This retinal deformation causes distorted vision, the main symptom of this subtype. Along with the accompanying decrease in visual acuity, the distortion can be very limiting.
The treatment consists of injections placed directly into the eye. These injections, called intravitreal injections, must be administered by a retina specialist. Currently, there are a few approved drugs for this disease (ranibizumab, aflibercept, faricimab and brolucizumab). The injections need to be given monthly during the initial months.
After the injections, we check if they were effective, whether more are needed, or if we can go a few months without any. If the lesion doesn’t return, we gradually increase the time between injections. As with dry AMD, we recommend home monitoring using the Amsler grid (you’ll find one at the end of the article).
In this way, wet AMD is transformed into dry AMD. As you’ll see, this is not a cure for the disease, but rather a way to slow down the rapid or aggressive version of it.