Syphilitic uveitis, DO NOT forget it!!
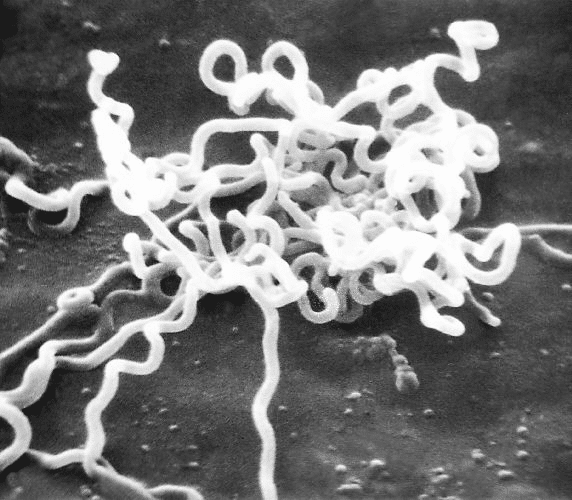
Syphilitic uveitis is an ocular manifestation of syphilis, an infectious disease caused by the bacterium Treponema pallidum. Although syphilis has been known for centuries, its ability to affect multiple body systems, including the eyes, remains a clinically relevant topic. Uveitis, which refers to inflammation of the uvea (the middle layer of the eye, including the iris, ciliary body, and choroid), can be a serious complication of syphilis and requires timely diagnosis and treatment to prevent irreversible ocular damage.
Contents
Epidemiology
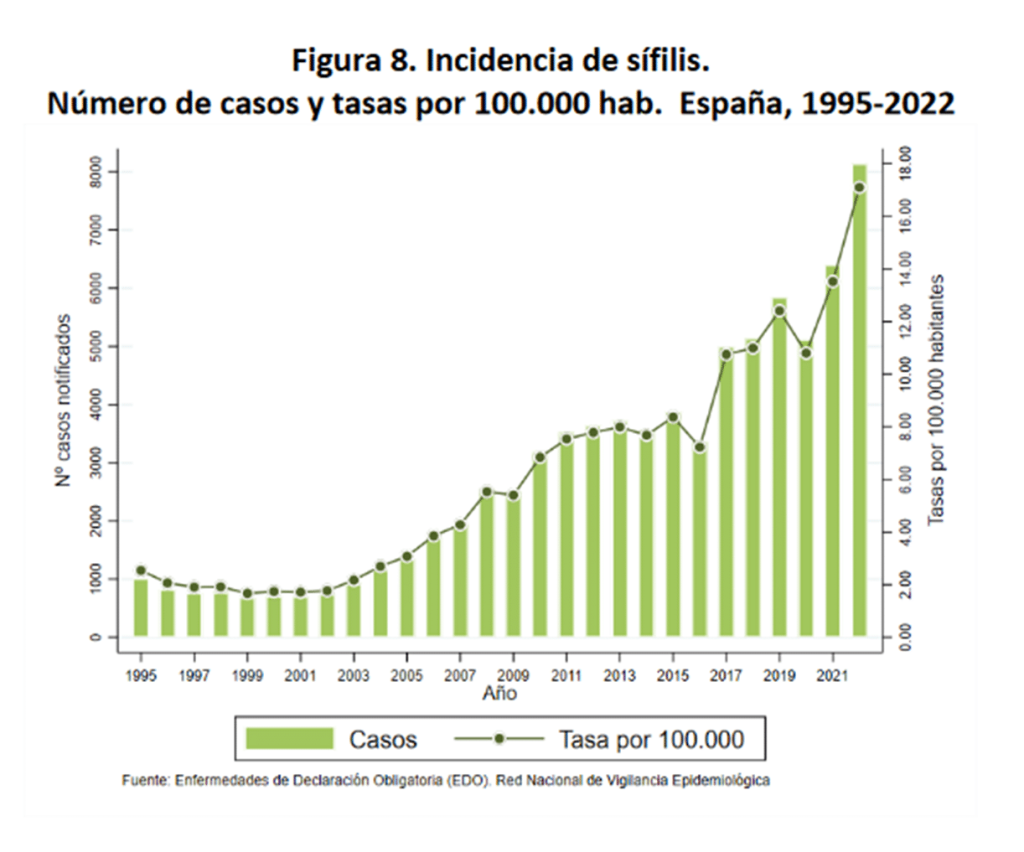
Syphilis is a sexually transmitted disease that has experienced fluctuations in incidence throughout history. Although the introduction of penicillin in the 20th century significantly reduced its prevalence, there has been a resurgence of cases in recent decades, particularly in populations with risk factors such as men who have sex with men (MSM), individuals with multiple sexual partners, and those infected with the human immunodeficiency virus (HIV). This increase in syphilis incidence has led to a parallel rise in associated complications, including syphilitic uveitis.
In fact, in our setting, the lowest historical rate of syphilis occurred in the 2000s, but since then, the numbers have continued to rise. As a notifiable disease, population data are available through the Ministry of Health. Approximately 35-40% of syphilitic uveitis cases are associated with HIV.
Syphilitic uveitis can occur at any stage of syphilis, although it is more common in the secondary and tertiary stages of the disease.
Pathogenesis
The pathogenesis of syphilitic uveitis is related to the ability of Treponema pallidum to spread through the bloodstream and affect multiple organs, including the eyes. The bacterium can invade ocular tissues, triggering an inflammatory response that leads to uveitis. In some cases, the inflammation may result from an immune reaction mediated by antigen-antibody complexes, contributing to tissue damage.
Clinical Forms
Ocular syphilis can manifest in various forms, including anterior uveitis, intermediate uveitis, posterior uveitis, or panuveitis (involving the entire uvea). Anterior uveitis, which affects the iris and ciliary body, is the most common form of syphilitic uveitis. However, inflammation can also extend to the choroid and retina, potentially leading to serious complications such as retinal detachment, macular edema, and optic atrophy.
As described by Furtado et al., syphilis can present as almost any type of ocular inflammation, from scleritis to neuroretinitis, so this etiology should always be considered.
There are three presentations in which syphilis should always be included in the differential diagnosis. Besides acute retinal necrosis, the following two presentations should be considered:
Acute Syphilitic Posterior Placoid Chorioretinitis
This condition is characterized by a relatively subtle hypopigmented macular lesion (bilateral or unilateral). When examining the fundus with high magnification, this lesion may go unnoticed.

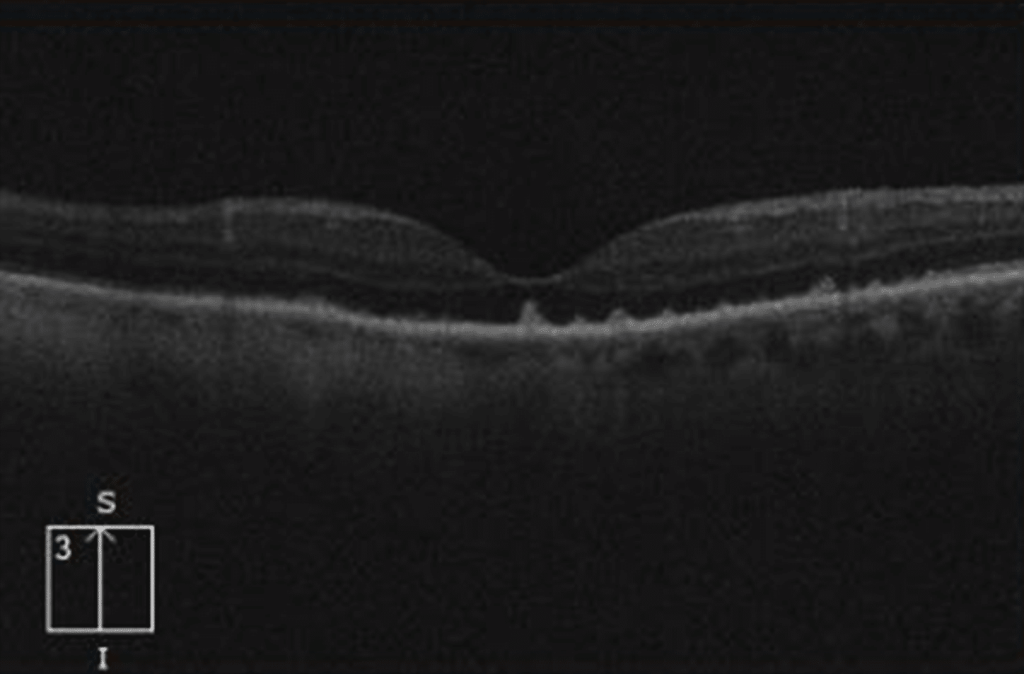
On OCT, finger-like projections are typically seen extending from the outer retinal layers to the inner layers.
On autofluorescence, a more or less rounded hyperautofluorescent lesion with an even brighter hyperautofluorescent halo is often observed.
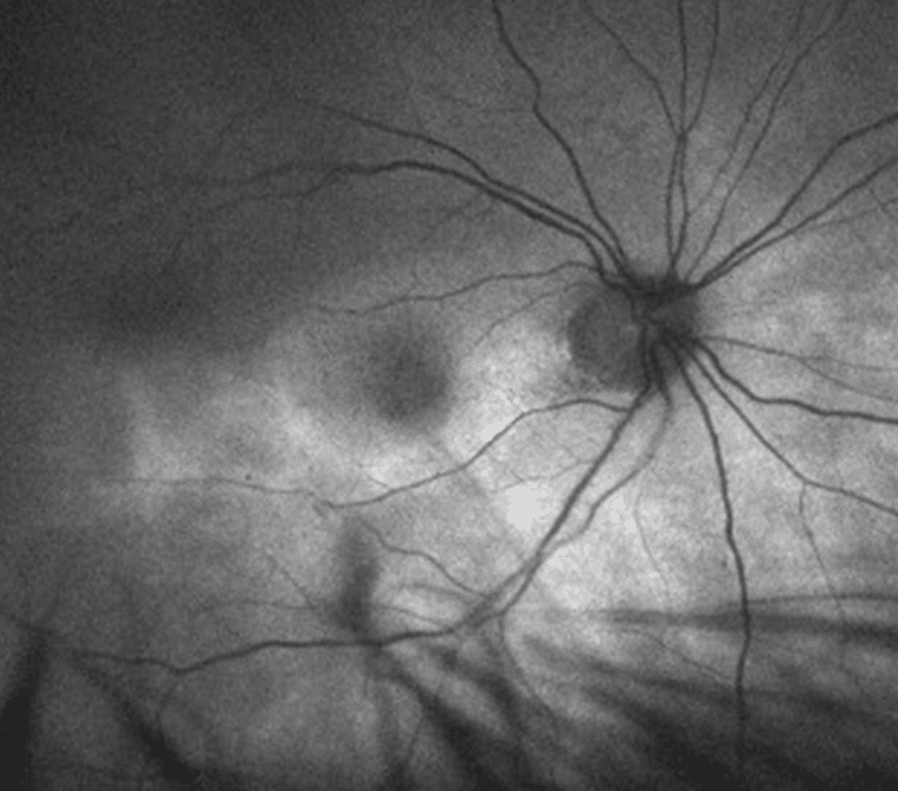
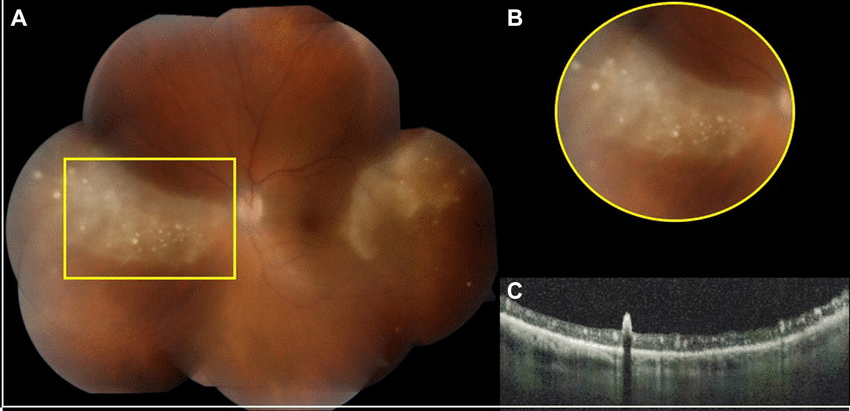
Peripheral Retinitis
This lesion usually presents bilaterally, typically in the temporal or nasal sectors, as a whitish triangular area. Over this lesion, which some authors describe as having a “ground-glass” appearance, whitish punctate lesions affecting the more superficial retinal layers may appear.
Diagnosis
The diagnosis of syphilitic uveitis requires a high index of suspicion, especially in patients with risk factors for syphilis. The initial evaluation should include a detailed clinical history, with emphasis on sexual history and the presence of systemic symptoms of syphilis, such as skin rashes, fever, or lymphadenopathy.
Diagnostic tests for syphilis include:
- Non-treponemal tests: These tests, such as VDRL (Venereal Disease Research Laboratory) and RPR (Rapid Plasma Reagin), detect non-specific antibodies produced in response to Treponema pallidum infection. Although useful for screening, they can yield false-positive results in certain conditions, such as autoimmune diseases or viral infections.
- Treponemal tests: These tests, such as FTA-ABS (Fluorescent Treponemal Antibody Absorption) and TP-PA (Treponema pallidum Particle Agglutination), detect specific antibodies against Treponema pallidum and are more specific than non-treponemal tests. A positive treponemal test confirms exposure to the bacterium.
The traditional algorithm involves performing non-treponemal tests first, followed by treponemal tests if the former are positive. The reverse algorithm, which has gained popularity in recent years, proposes the opposite order.
In cases of syphilitic uveitis, both the American CDC and various European societies recommend managing the patient under the assumption of neurosyphilis.
Treatment
The treatment of syphilitic uveitis focuses on eradicating Treponema pallidum with antibiotics and controlling ocular inflammation. The standard treatment for syphilis is penicillin, which remains the antibiotic of choice due to its efficacy against Treponema pallidum.
Given the potential for neurosyphilis, treatment is more aggressive than for forms without central nervous system involvement. In such cases, treatment involves intravenous Penicillin G sodium, 4 million units every 4 hours for 10-14 days.
For patients allergic to penicillin, alternatives such as doxycycline or ceftriaxone may be used, although penicillin remains the preferred treatment, and desensitization to penicillin is recommended.
In addition to antibiotic therapy, the management of syphilitic uveitis may require the use of topical or systemic corticosteroids to control ocular inflammation. In severe cases, immunosuppressants or biologic therapy may be necessary.
Prognosis
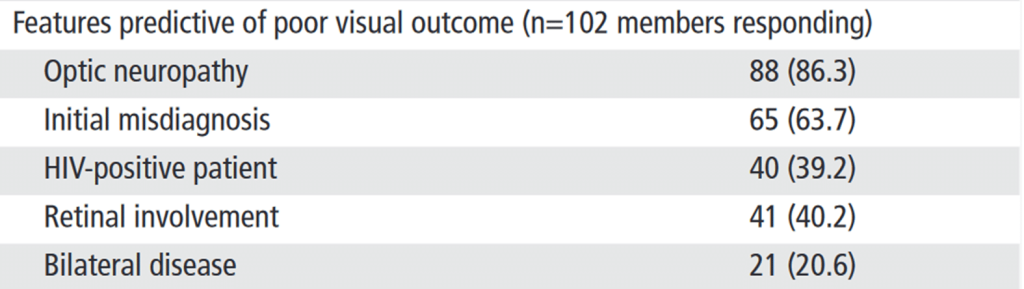
The prognosis of syphilitic uveitis depends on the timeliness of diagnosis and treatment. With appropriate treatment, most patients experience resolution of inflammation and improvement in visual acuity. However, in cases of delayed diagnosis or inadequate treatment, complications such as glaucoma, cataracts, retinal detachment, or optic atrophy may occur, potentially leading to permanent vision loss.
As you will see, delayed diagnosis due to initial misdiagnosis is the strongest predictor of poor final visual acuity.
Conclusion
Syphilitic uveitis is a serious ocular manifestation of syphilis that requires timely diagnosis and treatment to prevent irreversible visual complications. Ophthalmologists and physicians in general should maintain a high index of suspicion in patients with uveitis, especially those with risk factors for syphilis. Penicillin remains the cornerstone of treatment, and controlling ocular inflammation is essential to preserve vision. With a multidisciplinary approach involving ophthalmologists, infectious disease specialists, and primary care physicians, it is possible to improve outcomes in patients with syphilitic uveitis and reduce the burden of this disease in the population.
References
- Oliver, G. F. et al. Current ophthalmology practice patterns for syphilitic uveitis. Br J Ophthalmol 103, 1645–1649 (2019).
- Furtado, J. M. et al. Clinical Manifestations and Ophthalmic Outcomes of Ocular Syphilis at a Time of Re-Emergence of the Systemic Infection. Sci Rep 8, 12071 (2018).
- Ministry of Health. Epidemiological Surveillance of Sexually Transmitted Infections in Spain, 2022. (2024).